
Telemedicine: Capital Alpha Partners
Telemedicine. It is here to stay as it evolves from a mere replacement of in-person visits and it will continue to be the subject of regulatory framing at both the state and federal levels.
“First do no harm”
We should expect the funding and regulatory uncertainty around telehealth to continue for years. On the other hand, it is probably better that regulators proceed slowly instead of butchering it.
Rob Smith and the team at Capital Alpha Partners produced an excellent piece over the weekend reviewing the most recent medical utilization trends and what we should expect for the future. [For access to the complete report submit the form]
What you need to know:
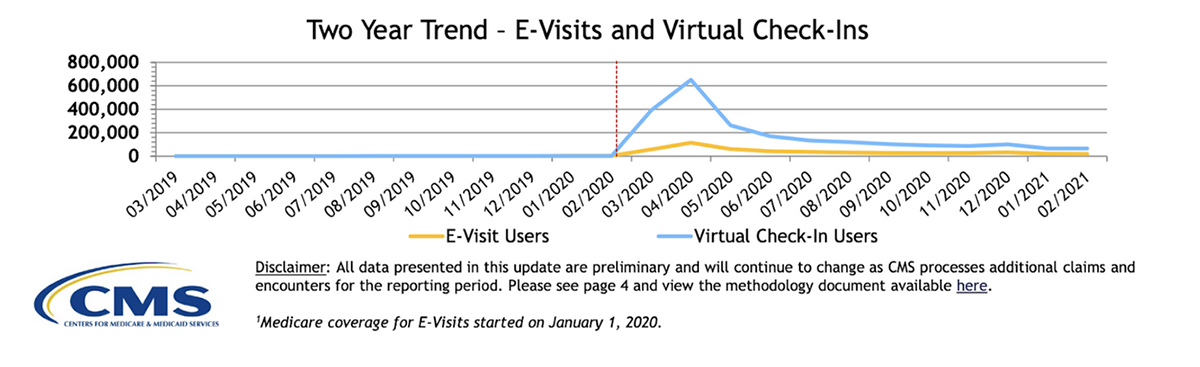
- Use: Telemedicine peaked at over 10 million episodes/month at the onset of the pandemic. And since then has stabilized at ~ 5 million/month.
- Permanence: Given the stability of that statistic it is likely CMS (the Center for Medicare & Medicaid Services) will extend the telehealth waiver program even after the public health emergency ends.
- Access: The demographics of the data show significant progress improving access to underserved populations. In particular Medicare-Medicaid dual eligibles were more likely to use telehealth services than traditional Medicare beneficiaries (62% to 50%).
The team at Capital Alpha believes:
“… it will be years before Congress will act on telehealth permanence in a meaningful way. In general, it takes roughly two years for CMS to generate a full year of spending and quality data, so it’ll be next year before we see a full picture of service use through the first year of the pandemic.”
While there is significant enthusiasm for creating a permanent policy for telemedicine, there’s also significant disagreement across the committees with jurisdiction. Expect the process to take some years to reach consensus and that waivers will be extended until that happens.

Washington, D.C.
Founded: 2007

